Page 9 - Venafi - 2021 Benefit Guide - CA
P. 9
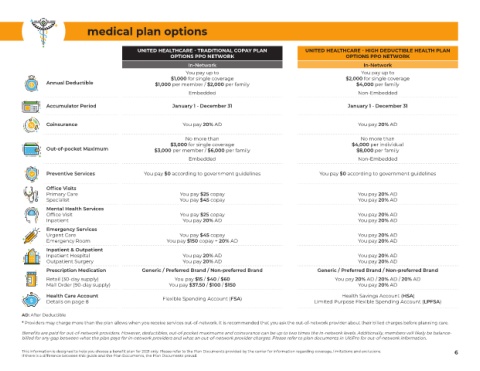
medical plan options
UNITED HEALTHCARE - TRADITIONAL COPAY PLAN UNITED HEALTHCARE - HIGH DEDUCTIBLE HEALTH PLAN
OPTIONS PPO NETWORK OPTIONS PPO NETWORK
In-Network In-Network
You pay up to You pay up to
$1,000 for single coverage $2,000 for single coverage
Annual Deductible $1,000 per member / $2,000 per family $4,000 per family
Embedded Non-Embedded
Accumulator Period January 1 - December 31 January 1 - December 31
Coinsurance You pay 20% AD You pay 20% AD
No more than No more than
$3,000 for single coverage $4,000 per individual
Out-of-pocket Maximum $3,000 per member / $6,000 per family $8,000 per family
Embedded Non-Embedded
Preventive Services You pay $0 according to government guidelines You pay $0 according to government guidelines
Office Visits
Primary Care You pay $25 copay You pay 20% AD
Specialist You pay $45 copay You pay 20% AD
Mental Health Services
Office Visit You pay $25 copay You pay 20% AD
Inpatient You pay 20% AD You pay 20% AD
Emergency Services
Urgent Care You pay $45 copay You pay 20% AD
Emergency Room You pay $150 copay + 20% AD You pay 20% AD
Inpatient & Outpatient
Inpatient Hospital You pay 20% AD You pay 20% AD
Outpatient Surgery You pay 20% AD You pay 20% AD
Prescription Medication Generic / Preferred Brand / Non-preferred Brand Generic / Preferred Brand / Non-preferred Brand
Retail (30-day supply) You pay $15 / $40 / $60 You pay 20% AD / 20% AD / 20% AD
Mail Order (90-day supply) You pay $37.50 / $100 / $150 You pay 20% AD
Health Care Account Flexible Spending Account (FSA) Health Savings Account (HSA)
Details on page 8 Limited Purpose Flexible Spending Account (LPFSA)
AD: After Deductible
* Providers may charge more than the plan allows when you receive services out-of-network. It is recommended that you ask the out-of-network provider about their billed charges before planning care.
Benefits are paid for out-of-network providers. However, deductibles, out-of-pocket maximums and coinsurance can be up to two times the in-network levels. Additionally, members will likely be balance-
billed for any gap between what the plan pays for in-network providers and what an out-of-network provider charges. Please refer to plan documents in UltiPro for out-of-network information.
This information is designed to help you choose a benefit plan for 2021 only. Please refer to the Plan Documents provided by the carrier for information regarding coverage, limitations and exclusions. 6
If there is a difference between this guide and the Plan Documents, the Plan Documents prevail.